The Increasing Ubiquity of Paracetamol Use During Labour: Promoting a Reassessment of Its Application
It has become a prevalent practice for women to receive the advice of taking two paracetamol when they reach out to the labour ward to notify midwives about the onset of early labour. The instruction, “Take two paracetamol and update us when your contractions are closer together,” has established itself as a standard recommendation over the past two decades. On the surface, this guidance might appear innocuous, but the observations made by The Undercover Midwife raise a thought-provoking perspective. Reflecting on her extensive experience, she remarks, “I just do not remember, either as an NHS or independent midwife in the 1980s and 1990s, women having such long exhausting and problematic latent phases as they do now. I also don’t remember anyone telling women to “take a couple of paracetamol”.
This prompts us to explore the possible complications that might arise from the seemingly innocuous use of this common drug. It is essential to approach the topic with a sense of awareness, as no drug can be entirely exempt from the potential for side effects. Assertions that any drug lacks side effects can be seen as either a manifestation of ignorance or an intentional misrepresentation. The truth is that all drugs carry inherent risks associated with their usage.
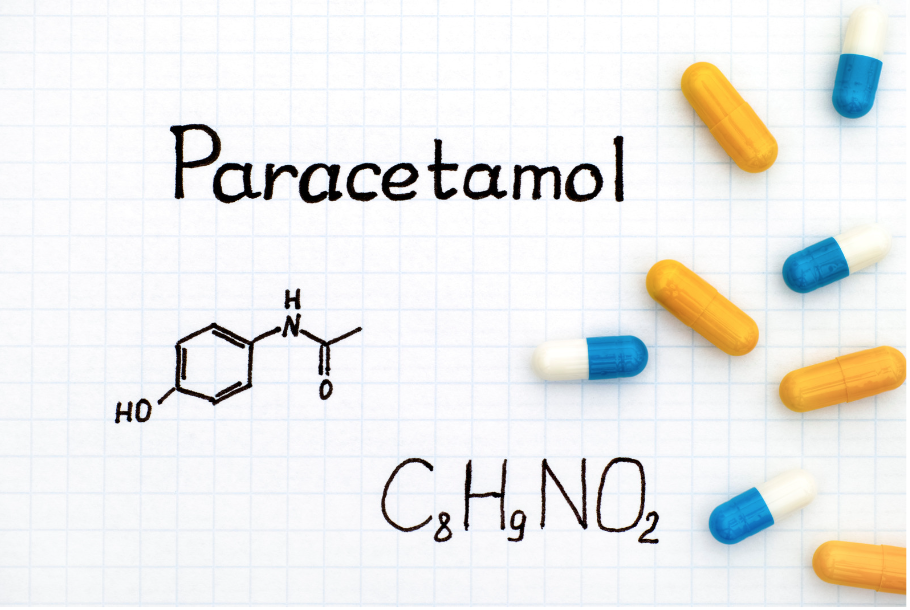
What is paracetamol?
Paracetamol is classified as an analgesic, which means it is a type of medication that is primarily used to relieve pain. It works by interfering with pain signals in the body and altering the way the brain perceives and responds to pain. The exact mechanism of how paracetamol produces its analgesic effects is not completely understood, but it is believed to involve several actions:
Prostaglandin Inhibition: Paracetamol is thought to work by inhibiting an enzyme called cyclooxygenase (COX), specifically COX-2, which is involved in the production of prostaglandins. Prostaglandins are chemical messengers that play a key role in transmitting pain signals and promoting inflammation. By reducing the levels of prostaglandins in the body, paracetamol helps to dampen the pain response. (We will look at why this can be an issue during labour)
Central Nervous System Impact: Paracetamol is thought to have an effect on certain areas of the brain that are involved in pain processing and perception. It may influence the brain’s pain-regulating centres, making them less sensitive to pain signals originating from the body.
Temperature Regulation: Paracetamol’s ability to influence the body’s temperature-regulating centre in the brain might also contribute to its pain-relieving effects. By reducing fever, which often accompanies illnesses and can contribute to discomfort, it indirectly helps alleviate pain.
As we delve into the implications of the routine paracetamol advice given during early labour, it becomes evident that the practice might warrant closer scrutiny. What are the underlying risks? How might this practice affect the course of labour and the well-being of both the mother and the child? Delving into these questions reveals the need for a more comprehensive evaluation of the recommendations provided to expectant mothers, as well as a reevaluation of the role of paracetamol in labour management.
In essence, while the suggestion to take paracetamol in early labour has become commonplace, the observations of seasoned midwives raise valid concerns about its potential impact. In light of this, it is crucial to acknowledge that all medical interventions, no matter how seemingly benign, should be approached with a critical mindset. The evolving landscape of maternity care demands that we continually reassess practices to ensure that the well-being of both mothers and infants remains at the forefront of our endeavours.
Prostaglandins and the Labour Process
Central to the process of childbirth are prostaglandins, bioactive lipid molecules that play a pivotal role in uterine contractions and cervical ripening. These compounds facilitate the transition from latent to active labour by orchestrating a cascade of events that culminate in a successful labour experience. Paracetamol, however, acts as an inhibitor of prostaglandin synthesis, particularly COX-2, which is responsible for the production of prostaglandin E. This inhibition could potentially disrupt the finely tuned hormonal balance required for labour progression.
Paracetamol’s Impact on Labour
The practice of advising women to consume paracetamol during the latent phase of labour raises compelling concerns. Anecdotal evidence has highlighted instances where women have ingested substantial amounts of paracetamol. Despite the lack of systematic recording or analysis of these occurrences, the implications for both maternal health and foetal development cannot be ignored.
Unintended Consequences for Fetal Health
Research suggests that the use of paracetamol during pregnancy may be associated with undesirable outcomes. For instance, studies have found correlations between maternal paracetamol consumption and conditions like crypto-orchidism (undescended testes), childhood asthma, and even attention-deficit hyperactivity disorder (ADHD) in offspring. These findings raise legitimate concerns about the potential long-term effects on the health and well-being of the next generation.
The Balancing Act of Coping Mechanisms
The growing trend of extended latent phases has prompted the development of self-comforting and self-medicating strategies. These measures, designed to prevent early hospital admission, often include paracetamol alongside practices like warm baths, massage, and relaxation techniques. While some of these approaches have merit, the widespread and unexamined use of paracetamol presents a potential conflict between immediate relief and the natural course of labour.
The Call for Critical Evaluation
The prevailing practice of suggesting paracetamol usage during labour necessitates reevaluation. Healthcare professionals must consider the possible ramifications of advising a drug that interferes with the delicate hormonal symphony that propels labour. A comprehensive investigation into the effects of paracetamol on labour dynamics, maternal physiology, and fetal development is urgently needed.
Balancing Care and Evidence-Based Practice
As the medical community strives to offer women the best possible care during childbirth, it is essential to assess and adjust the practices that have become normalised. Ensuring that medical advice aligns with the goals of safe, effective, and healthy childbirth is paramount. The role of paracetamol during labour deserves rigorous scrutiny and exploration to safeguard both maternal well-being and the future health of our offspring.
In conclusion, while paracetamol has long been considered a reliable analgesic, its use during the latent phase of labour requires careful consideration. As we navigate the complex landscape of modern obstetrics, a thoughtful approach to medication recommendations and evidence-based practices will ultimately contribute to a safer and more positive labour experience for women and their newborns.
Discover a Holistic and Thought-Provoking Childbirth Course: Embrace a Fulfilling Journey of Self-Employment While Nurturing Women Through Pregnancy, Birth, and Beyond. Break Away from Conventional Clinical Training and Explore a Comprehensive One-Year Program that Cultivates Critical Thinking. Embark on the Path of Empowerment and Autonomy for Birthing Mothers. Join Us Today for a Course that Resonates with Your Passion and Drives Your Entrepreneurial Spirit!