Why does pre eclampsia occur and how can we prevent it?
In the 1950s and 1960s, Dr. Tom Brewer, an obstetrician, made a significant discovery regarding the cause of pre-eclampsia. Through extensive research on the works of previous doctors like Hamlin, Strauss, Burke, and Ferguson, who had studied the issue for four decades, Dr. Brewer found that pre-eclampsia was linked to abnormal blood volume resulting from malnutrition or food deficiency.
During pregnancy, one of the crucial roles of the body is to support the pregnancy and nourish the developing baby. The body’s effectiveness in achieving this largely depends on its ability to increase the mother’s blood volume. Typically, the blood volume is expected to increase by 50-60% throughout the pregnancy.
To facilitate this blood volume expansion, the liver produces a substance called albumin, which has properties similar to egg whites. When present in the mother’s bloodstream, albumin generates osmotic pressure, helping to draw excess fluid from her tissues back into her blood vessels. However, the liver can only produce albumin from protein that the mother consumes.
A key issue arises when pregnant women try to limit their weight gain to conform to an “ideal” number by following high protein but low-calorie diets. In such cases, much of the protein intake is used for energy, leading to a deficiency in albumin production. Dr. Brewer’s research indicates that when a woman consumes around 1/3 less than the recommended 2600 calories, approximately 1700 calories, half of the protein she ingests will be burned for energy. Consequently, only 60 out of her 120 grams of protein would be available for albumin production, along with the development of baby cells and uterine muscle cells. This deficiency in albumin can likely hinder her ability to adequately expand her blood volume during pregnancy.
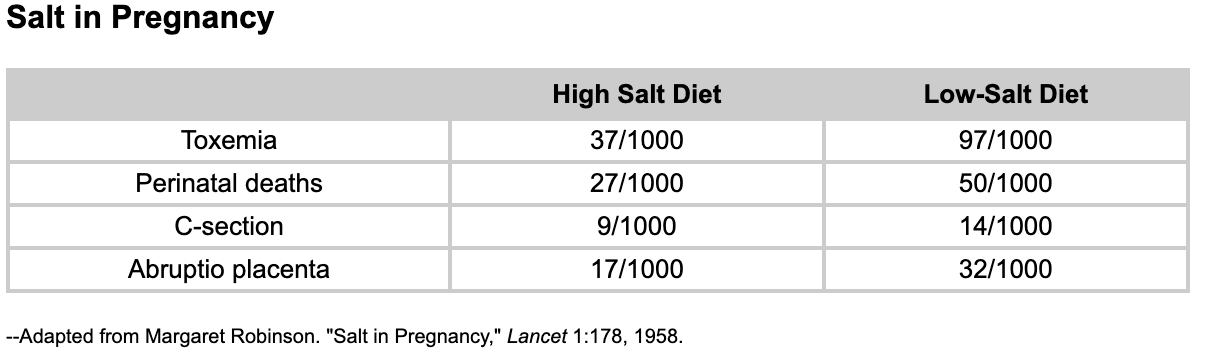
Salt also plays a role in osmotic pressure, aiding in the removal of excess fluid from tissues and promoting circulation. While limiting salt intake may be beneficial for pregnant women with underlying heart or kidney conditions, it can be risky for healthy women. Generally, a healthy woman’s taste buds serve as an accurate indicator of her salt needs, and research suggests that it is unlikely for a healthy pregnant woman to consume excessive salt. Her kidneys naturally eliminate any extra salt she ingests. Moreover, studies have demonstrated that after only two weeks of practicing “salt in moderation,” a decrease in the mother’s blood volume occurs.
When the blood volume stops increasing or decreases during pregnancy, the body’s response mechanism can be mistaken. Instead of recognising that the mother is consuming less food, it interprets the decreased blood volume as a potential haemorrhage situation. As a result, the body initiates processes similar to those used during actual haemorrhages. The kidneys release an enzyme called renin, causing the blood vessels to constrict. This natural response, useful during haemorrhage to redirect blood to vital organs, leads to an increase in blood pressure during pregnancy.
Trying to address this rising blood pressure by restricting salt or weight only exacerbates the situation. It further reduces blood volume, leading to more renin production and additional blood vessel constriction, resulting in further elevation of blood pressure.
Concurrently, the kidneys strive to augment blood volume by reabsorbing as much water and salt as possible from the filtered fluid. However, due to insufficient albumin and salt in circulation to hold the reabsorbed water, much of it leaks into the tissues. This process leads to rapid swelling in the ankles and rapid weight gain as the excess water accumulates in the mother’s tissues.
The pregnant woman seeks medical attention from her birth attendant, who diagnoses her with developing pre-eclampsia. If her nutritional status is not promptly improved, her blood volume will continue to decrease, and she may progress to eclampsia (toxemia). Toxemia can have severe consequences, including convulsions, coma, and even death. Some sources claim that the cause of toxemia remains unknown, leading many practitioners to address the symptoms without success. As a result, the symptoms persist, and the mother may experience a series of complications.
Treating Pre-eclampsia and Optimising Diet during Pregnancy
To address pre-eclampsia, one effective approach is to educate the mother about the underlying cause and encourage her to follow the Brewer Diet plan. The Brewer Diet recommends regular intake of protein-rich foods throughout the day, with the goal of consuming something containing protein every waking hour. This approach helps in maintaining adequate blood volume and supporting the pregnancy.
In cases where a more immediate response is required, the birth attendant may administer albumin intravenously to boost blood volume. Antibiotics may also be prescribed to reduce the burden on the liver from aromatic toxins present in the intestines. A story is shared of a woman who, unable to receive IV albumin, managed to lower her blood pressure by consuming a substantial amount of protein-rich foods, like 52 eggs and 6 quarts of milk, over three days.
Anne Frye recommends a tailored approach to protein intake, depending on the individual’s health history and pregnancy circumstances. For instance, if the woman has a history of liver disorders, a more cautious approach to protein intake is advised to avoid overwhelming the liver. Monitoring the mother’s lab work closely for changes is essential in such cases.
It is important to note that certain mainstream obstetric and perinatology practices, including anti-hypertensive drugs, may have adverse effects on the mother’s blood volume and liver function. Liver compromise can hinder the production of sufficient albumin required to support blood volume expansion during pregnancy, and it can also affect the body’s clotting mechanisms.
To prevent or manage rising blood pressure, edema, pre-eclampsia, IUGR (Intrauterine Growth Restriction), premature labor, or HELLP syndrome, a Brewer Diet counselor can work closely with the mother to assess her lifestyle and diet for potential adjustments. For instance, if the mother experiences salt and calorie losses, she can reduce exercise, work hours, and exposure to heat while increasing salt, calorie, and protein intake.
In specific situations, it is advisable to increase diet intake by adding 200 calories and 20 grams of protein. These situations include vomiting beyond the third month of pregnancy, pregnancies spaced less than a year apart, a previous pregnancy with adverse outcomes (low birth weight, neurologically handicapped, or stillborn child), a history of recurrent miscarriages or toxemia, failure to gain ten pounds by the twentieth week of pregnancy, serious emotional problems, working full-time at a demanding job, breastfeeding an older baby during pregnancy, and multiple pregnancies (twins or more).
References – The Complete Pregnancy Diet: Meeting Your Special Needs” from the book “Eating for Two” by Isaac Cronin and Gail Sforza Brewer
http://www.drbrewerpregnancydiet.com/id36.html




